Research in the field of cancer immunotherapy increasingly demonstrates the value of studying circulating immune cells in peripheral blood to identify new therapeutic targets to enhance tumor-killing immune responses. Here we highlight a handful of impactful publications in this field and provide a strategy for implementing peripheral immune profiling in your research and drug development pipeline.
Page Anchor: #wu-2022 – Not Visible On Front Fresh T cells from Blood Replenish Exhausted T Cells in Tumor to Sustain a Tumor-Killing Response
If tumor killing by immune cells happens at the tumor site, what is the role of the peripheral immune response in the effectiveness of immunotherapy treatments? Wu et al. address this important question in a Nature 2020 article.1 Cancer cells hide from immune cells using checkpoint proteins, such as PD-L1, that keep immune cell responses “in check.” Anti-PD-L1 monoclonal antibodies and others prevent cancer cells from doing this; they form a class of drugs known as immune checkpoint inhibitors.
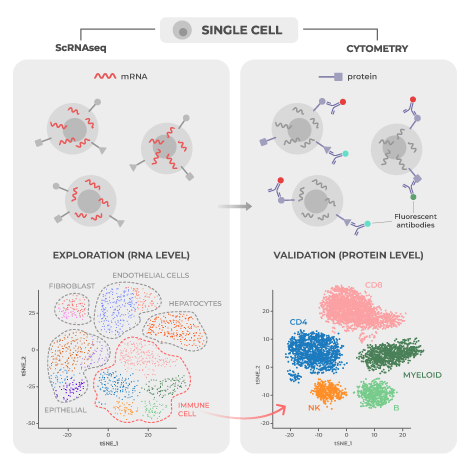
The researchers used deep single-cell sequencing of RNA and T cell receptors to analyze the characteristics of different populations of T cells and T cell receptors in tumors, normal tissue next to the tumor (normal adjacent tissue), and peripheral blood. Using these methods, the study authors were able to identify the location of targeted clonal expansion (replication of identical cells, called clones) of effector-like T cells, the specific subset of T cells that have direct anti-tumor activity. Targeted clonal expansion within peripheral blood predicted local clonal expansion both within the tumor and in normal adjacent tissue at the same time, which was associated with the drug working better.
Data both from this study and others indicate that non-exhausted T cells (T cells that are fully functional and active) and T cell clones that travel from the periphery to the tumor play a central role in patients’ ability to fight off tumors after receiving immune checkpoint inhibitors. Thus, identifying and analyzing tumor-killing T cells in peripheral blood samples is not only convenient but critical to drug discovery. Therapeutic breakthroughs may be missed if peripheral blood analysis is ignored.
Page Anchor: #spitzer-2017 – Not Visible On Front Reinforcements Needed: Effective Therapy Requires Immune Cells from Outside the Tumor
Teiko Bio’s cofounder Matt Spitzer and colleagues have published multiple studies demonstrating the importance of the peripheral immune response in cancer biology. In these studies, the research was carried out using mass cytometry, an advanced technique that expands on flow cytometry technology by using metal-tagged antibodies. Given the distinct characteristics of the metals used, mass cytometry has the capacity to detect more than 40 cellular markers simultaneously.
Prior to the publication by Wu et al., work by Spitzer et al. provided evidence that the peripheral immune system is the source of a prolonged and sustained tumor-killing response in their 2017 Cell paper.2 Using mass cytometry, the study authors investigated immune activity in a mouse model of triple-negative breast cancer following treatment with either a successful or unsuccessful immunotherapy.
The investigators found evidence of immune activity throughout the mouse’s body, not just in the tumor microenvironment. During the period of tumor rejection, eight days after giving a successful therapy, only peripheral immune cells, such as those from draining lymph nodes, spleen, peripheral blood, or bone marrow, exhibited a higher level of activity and replication (production of new cells). Furthermore, a specific subset of peripheral CD4+ T cells arose that provided immunity against new tumors, and their numbers grew in mice who responded to therapy. This peripheral immune activation was specific to successful therapy, as the peripheral immune cells of mice given an ineffective therapy showed very few immune differences when compared to untreated mice.
Overall, these findings suggest that a coordinated response engaging the entire immune system throughout the body is necessary to mount a persistent and effective tumor-killing response during treatment; simply activating immune cells within the tumor site is not enough. Since peripheral blood samples provide information on the systemic immune response critical for developing effective immunotherapies, they should not be overlooked.
Page Anchor: #allen-2020 – Not Visible On Front Cancer’s Impact on the Immune System Goes Beyond Tumor-Killing
A 2020 study published in Nature Medicine by Allen et al. explored how cancer alters systemic immune response to infection.3 Eight mouse strains bioengineered to develop tumors across five tissue types were investigated. In all mice studied, cancer development caused marked changes in systemic immunity; similar findings were demonstrated using gene expression data of breast cancer patients from the Norwegian Women and Cancer Study. In the mice, the immune cell changes in peripheral tissues were distinct from those in the tumor microenvironment.
The presence of tumor in the mouse models weakened the immune response to infectious disease. This manifested in many ways, including decreased T cell activity to fight off infections from viruses or bacteria. Investigators discovered that T cell activity could be restored by supercharging the response of another type of immune cell, called the antigen-presenting cell. When tumors were surgically removed, the healthy baseline functioning of the entire immune system was reestablished. Antibody blockade of specific immune signaling molecules (IL-1 and G-CSF) alone prevented many of the negative tumor-induced changes to overall immune function. This shows the importance of these signaling molecules to how the immune system dynamically changes and adapts to its environment. Results from this study provide convincing evidence that dynamic restructuring of the entire immune system, both in terms of composition and function, occurs in response to cancer.
Page Anchor: #shen-2021 – Not Visible On Front Peripheral Immune Profiling in Practice
How the immune system interacts with different types of cancer is now being studied for its potential as a predictive biomarker of response to treatment. Evidence for specific immune cell types guiding cancer progression, both positively or negatively, continues to build. A 2021 study by Shen et al. published in Science Translational Medicine found that certain immune protein identifiers (one of which is called lymphocyte-activation gene 3 or LAG-3 for short) on specific T cells (CD8+ T cells) predicted which patients would respond to immune checkpoint inhibitors.4 The researchers used flow cytometry to evaluate many different immune cell markers and the results were confirmed in two different patient data sets, one with melanoma (188 patients) and another with urothelial cancer. Both melanoma and urothelial cancer patients that had low levels of the LAG-3 immune biomarker on their CD8+ T cells were much more likely to respond to treatment.
A 2020 review paper published in Nature Reviews Cancer by Bruni, Angell, and Galon provides an outline of the primary immune factors that lead to tumors growing or shrinking.5 The importance of how the immune cell interacts with tumors can be seen in how checkpoint inhibitors work. If a robust adaptive anti-tumor immune response does not already exist before treatment, checkpoint inhibitors will be ineffective. There are many different cancer types, each having its own distinctive interactions with the immune system with many moving parts. Given this complexity, the authors of the review suggest that being able to predict how cancer patients respond to treatment can be improved by evaluating multiple immune parameters instead of relying on just one.
Page Anchor: #hartmann-2019 – Not Visible On Front What to Look For When You Don’t Know What You’re Looking For
An article published in Cell Reports in 2019 explored the power of mass cytometry to overcome investigator bias and ensure detection of unexpected cellular activities in clinical trials.6 These unforeseen activities might provide the key to a therapeutic breakthrough even for trials with limited sample sizes. The study authors created a standardized, comprehensive reference panel of 33 antibodies that covers all major immune cells subsets in the innate and adaptive immune system, while also quantitatively measuring markers of activation and immune checkpoint molecules in one assay.
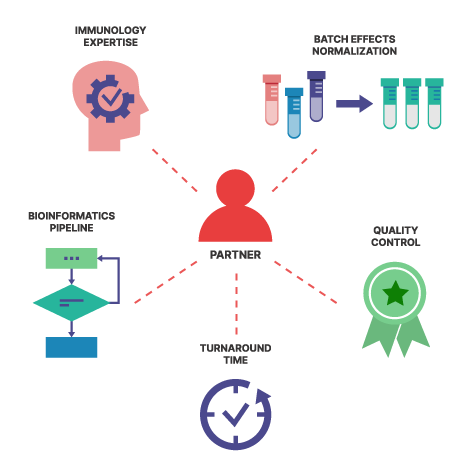
The mass cytometry panel was able to categorize at least 98% of peripheral immune cells, with each cell population expressing four or more antigens. The strength of the technique was demonstrated in its ability to produce consistent results across two research centers and different sample types, including peripheral blood samples, metastatic lymph node samples, and tumor biopsies. The investigators were able to characterize disease-associated immune signatures following bone marrow transplantation in leukemia patients who developed graft-versus-host disease compared to those who did not using their standardized 33 antibody reference panel. This published work formed the initial foundation for Teiko’s TokuProfile base panel, which was later optimized to add up to 12 additional open channels for customization.
In summary, a growing body of evidence suggests that not only can studying immune system changes in peripheral blood in clinical trial cancer patients result in important insights , but peripheral immune responses are key to finding immunotherapy breakthroughs. High-dimensional techniques such as mass cytometry, with its ability to gather data on the entire immune landscape at once, are leading the charge and helping researchers find clinically relevant biomarkers today.